What Is the Best Hydrocephalus Treatment?
WHAT IS HYDROCEPHALUS?
Hydrocephalus has been commonly called “water on the brain” or “fluid on the brain.” The water in reference here is actually cerebrospinal fluid (CSF), which has pooled in the brain due to an imbalance in the amount produced vs. the amount the body can absorb. Normally, CSF continuously flows through brain cavities called ventricles and the spinal cord, acting as a shock absorber and delivering vital nutrients before being absorbed into the bloodstream. Hydrocephalus interrupts this healthy flow of CSF, causing an accumulation that puts pressure on the brain.
Hydrocephalus can be either congenital – present before birth – or acquired, which develops after birth. There are two types: communicating and non-communicating. In a case of communicating hydrocephalus, CSF is blocked after leaving the brain’s ventricles. Non-communicating cases involve a blockage between one ventricle and another.
WHAT CAUSES IT?
According to the National Institute of Neurological Disorders and Stroke, one to two out of every 1,000 people is born with hydrocephalus. Although the exact cause isn’t always evident, it can stem from genetic abnormalities or developmental disorders. This can lead to complications and symptoms well into adult life. Acquired hydrocephalus, on the other hand, can result from a traumatic head injury, infection like meningitis, brain tumors, or a ruptured aneurysm.
Normal pressure hydrocephalus (NPH) is a type that occurs more frequently in the elderly and causes cognitive difficulties commonly misdiagnosed as Alzheimer’s. The Hydrocephalus Association website states that “more than 700,000 Americans have NPH, but less than 20% receive an appropriate diagnosis.” For this reason, it’s essential to consult expert physicians with extensive experience diagnosing NPH, like those at IGEA. Usually, this type of hydrocephalus is caused by injury, infection, tumor, or inflammation.
WHAT ARE HYDROCEPHALUS SYMPTOMS?
Hydrocephalus manifests differently depending on the cause and type. Symptoms commonly found in young adults include:
- Chronic headaches
- Blurred or double vision
- Difficulty walking
- Impaired bladder control
- Memory loss
- Vomiting, nausea, drowsiness
Later in life, normal pressure hydrocephalus may affect the neurological areas that control the legs and bladder, along with cognitive processes, causing:
- Dementia (affecting memory, concentration, and interest in daily activities)
- Difficulty walking
- Urinary incontinence
HOW IS HYDROCEPHALUS TREATED?
There are a few prevailing methods, each one appropriate for different situations. But by addressing it early, a patient can fully recover with no future complications.
ENDOSCOPIC THIRD VENTRICULOSTOMY
The primary alternative to shunt systems, the primary goal of endoscopic third ventriculostomy (ETV) is to eliminate a patient’s shunt dependency. This minimally-invasive procedure uses an endoscope to release CSF buildup by puncturing the third ventricle, allowing fluid to bypass the obstruction and flow freely around the surface of the brain, reabsorbing as it should.
Shunts have proven effective in a variety of cases, but studies show that ETV can deliver a 65-70% success rate in cases of shunt malfunction. It’s a one-time procedure, where shunts often require ongoing maintenance, and it can be preferable in cases involving an obstruction like a tumor. Plus, it keeps all of your CSF around the brain and spinal cord without diverting it to other parts of the body.
MEDICATIONS
Certain medications, specifically Acetazolamide and furosemide, appear to reduce CSF levels by acting on the choroid plexus, the intraventricular tissue that produces this fluid. However, relying solely on medication to treat hydrocephalus is a controversial topic, and it’s better used temporarily, or in cases when other procedures aren’t possible.
So, which one is best? There isn’t one overarching answer. It completely depends on your age, health, prior surgeries, and other factors. The most common and well-documented are shunt systems, but in certain cases (like obstructive hydrocephalus), ETV may be a better option. In the end, it’s up to you and your physician to evaluate a menu of treatments and determine which one is best for your unique circumstances.
WHAT CAUSES IT?
According to the National Institute of Neurological Disorders and Stroke, one to two out of every 1,000 people is born with hydrocephalus. Although the exact cause isn’t always evident, it can stem from genetic abnormalities or developmental disorders. This can lead to complications and symptoms well into adult life. Acquired hydrocephalus, on the other hand, can result from a traumatic head injury, infection like meningitis, brain tumors, or a ruptured aneurysm.
Normal pressure hydrocephalus (NPH) is a type that occurs more frequently in the elderly and causes cognitive difficulties commonly misdiagnosed as Alzheimer’s. The Hydrocephalus Association website states that “more than 700,000 Americans have NPH, but less than 20% receive an appropriate diagnosis.” For this reason, it’s essential to consult expert physicians with extensive experience diagnosing NPH, like those at IGEA. Usually, this type of hydrocephalus is caused by injury, infection, tumor, or inflammation.
WHAT’S THE OUTLOOK FOR PATIENTS?
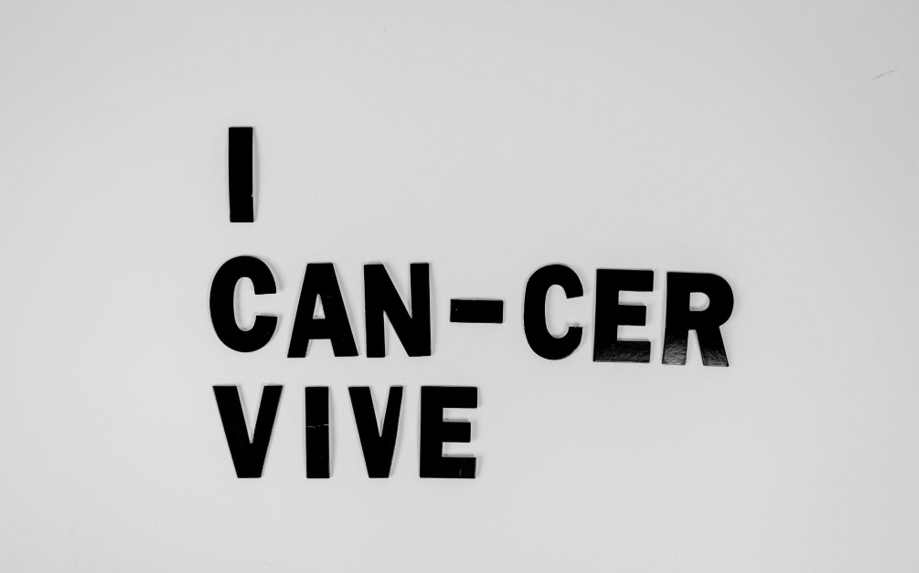
If addressed early and with the appropriate treatment, hydrocephalus has a fairly high survival rate. Many patients go on to live long and unrestricted lives, like those profiled on the Hydrocephalus Association website. Shunt treatment can even reverse the symptoms of dementia in elderly patients. Unfortunately, hydrocephalus isn’t something that disappears on its own, so it’s crucial that you schedule a doctor’s appointment and get the necessary treatment if you begin exhibiting symptoms.
The neurosurgeons at IGEA are caring experts, well-versed in the most advanced treatments. With extensive experience treating neurological conditions, your diagnosis and treatment couldn’t be in better hands. Contact us to schedule a consultation appointment today.