Pituitary Tumors: New Jersey Neurosurgeons Describe the Symptoms and Explain the Latest Treatment Approaches
“You have a tumor on a gland at the base of your brain.” It’s news that more than 10,000 Americans receive each year, and this diagnosis of a pituitary tumor often is, understandably, cause for considerable anxiety. The board-certified neurosurgeons of IGEA Brain, Spine & Orthopedics have extensive experience providing patients with education to allay that anxiety, as well as with minimally invasive surgical care to address the symptoms the tumors can cause. Those neurosurgeons – David Poulad, MD, FAANS, FACS; Adam Lipson, MD, FAANS, FACS; Ciro G. Randazzo, MD, MPH, FAANS; and Anil Nair, MD, FAANS – routinely perform highly sophisticated procedures to remove pituitary tumors at tertiary neurosurgical centers including Overlook Medical Center, Morristown Medical Center, St. Barnabas Medical Center, and St. Joseph’s Regional Medical Center. In a recent interview, Dr. Lipson and Dr. Nair reviewed the key points they share with patients and the latest operative techniques they employ in treating pituitary tumors.
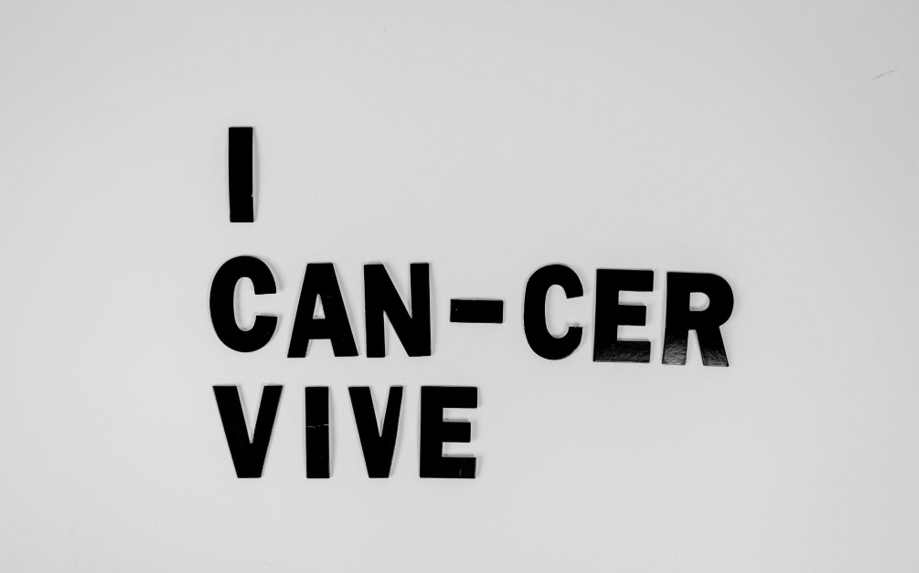
“One of the most important things to know about pituitary tumors is that the great majority are not cancerous,” Dr. Lipson says. “They can still cause significant problems by interfering with hormone levels or pressing on adjacent tissues and structures, but we want people to understand that in most cases these tumors are benign, and do not represent cancer.” He adds that the tumors are found in women and men in equal measure, are not more or less common in any particular ethnic or racial group, and can affect children as well as adults, although they most commonly are diagnosed in the third and fourth decades of life.
Dr. Nair notes, “While people usually have heard of the pituitary gland, many are not familiar with its function or location. So we also spend time describing the gland’s role – as this helps explain the symptoms that a pituitary tumor can cause — and its location, which is a major consideration in our surgical approach.” Dr. Nair adds that the pituitary is considered the body’s “master gland” because the hormones it produces affect many functions, including growth and reproduction, while also controlling other glands and the hormones they secrete. He continues that the pituitary gland, which is roughly the size of a pea, is located at the base of the brain.
Dr. Lipson says, “Because the gland affects so many aspects of the body and health, the symptoms of a pituitary tumor can be quite varied. Those symptoms can reflect over-secretion or under-secretion of hormones, such as thyroid problems, abnormal nipple discharge, changes in energy level, or changes in skin, facial features, or finger size.” He adds that these hormonal imbalances also can affect fertility and menstruation. In other cases, Dr. Lipson notes, as a tumor grows and compresses surrounding structures such as the sinuses or optic nerve, it can cause headaches or visual problems.
Initial steps in diagnosing a pituitary tumor depend on the patient’s symptoms, Dr. Nair says. In some instances, those symptoms are common and non-specific, meaning that they potentially could represent a wide variety of causes, such as is the case with headaches and low energy levels.
In other situations, while a number of conditions might be responsible for the symptom, the choice of initial evaluations is clear. For example, when a patient is experiencing changes in her menstrual cycle or difficulty becoming pregnant, checking hormone function is a standard first step, while visual problems are evaluated through a comprehensive ophthalmologic examination and, often, magnetic resonance imaging (MRI).
In still other scenarios, the nature of the symptom causes physicians to focus on pituitary issues early in the evaluation process. “For example, when a person presents with nipple discharge, physicians will consider the possibility of a prolactinoma, which is a pituitary tumor that produces an excess amount of the hormone prolactin. In other cases, a person will note that his or her glove, shoe, or hat size is increasing. This will prompt a doctor to think in terms of a possible pituitary tumor that is secreting growth hormone,” Dr. Nair notes. In making the diagnosis, key factors include altered blood hormone levels or abnormal findings on an ophthalmologic examination, as well as the results of a CT scan or an MRI of the brain in which a contrast agent is used to visualize the tumor.
Once a pituitary tumor has been identified, the choice of treatment depends on several factors, says Dr. Lipson, whose practice focus is on brain tumors, pituitary tumors, and minimally invasive spinal surgery techniques. “In some cases, the person had no symptoms at all, and the tumor was found on a CT scan or MRI performed for another reason,” he notes, adding that as many as 1 in 4 people may develop a pituitary tumor over the course of their lives, with the majority of those people experiencing no symptoms. He adds that non-symptomatic tumors that are not compressing the optic nerves do not require immediate intervention, and that a neurosurgeon instead can monitor the patient over time.
When patients are experiencing symptoms, the type of tumor helps determine treatment, notes Dr. Lipson. He explains that medication typically is the first-line therapy for prolactinomas, while surgery generally is the preferred initial approach for other tumors, particularly if there is compression of the optic nerve or if a tumor is secreting growth hormone or adrenocorticotropic hormone (ACTH). Meanwhile, radiosurgery techniques may be employed for tumors invading the cavernous sinus or that have recurred, he adds.
“Recent years have seen significant advances in the surgical management of pituitary tumors, and all of the neurosurgeons at IGEA have extensive experience performing transnasal, transsphenoidal surgery to remove these tumors,” Dr. Lipson says, referring to a technique in which surgeons carefully guide small instruments through the nostril and sinus cavity to reach the pituitary gland. He continues, “We perform endoscopic or microscopic surgery using computer navigation to remove the tumor in the least invasive manner possible, with the surgical strategy individualized to each patient’s specific situation.”
Dr. Lipson adds that patients generally spend 1 to 3 days in the hospital after the procedure. “Patients are generally very pleased with the outcome of this surgery,” the neurosurgeon says.
Dr. Nair notes, “Following surgery, it is not uncommon to have some initial nasal irritation that improves over time. Because the pituitary controls the hormones in the body, we will need to monitor your labs in the hospital until they have stabilized, but the majority of people do not have long-term hormonal effects. That being said, we work closely with the endocrinology team to make sure you are safe and healthy before going home.”
“Being told that you have a pituitary tumor obviously can be very disconcerting, but when people learn that these tumors overwhelmingly are benign and can be treated safely and effectively, that initial anxiety hopefully abates very quickly,” says Dr. Nair, who completed a fellowship in neurovascular surgery and endovascular surgery at Jefferson Hospital for Neuroscience in Philadelphia. He also completed an enfolded year of endovascular neurosurgery, a neurosurgery residency, and a general surgery internship at Albany Medical Center. He received his medical degree from the University of Missouri-Kansas City School of Medicine.
Dr. Lipson says that IGEA’s physicians are able to provide New Jersey residents with effective, minimally invasive treatment of pituitary tumors without those people having to travel to Manhattan, Philadelphia, or more-distant cities. “We have extensive experience in brain and pituitary tumor surgery individually tailored to each patient, with the surgeries all performed by board-certified neurosurgeons with between 13 and 25 years’ experience in the surgical management of these tumors. We offer outcomes that are equal or superior to those of any academic medical center,” says the neurosurgeon, who received his medical degree with honors from Harvard Medical School in 2000 and then continued his training with neurosurgical residencies at the University of Washington and Penn State Hershey Medical Center in Hershey, PA.
As noted, the IGEA team of board-certified neurosurgeons treating pituitary tumors includes Dr. David Poulad and Dr. Ciro G. Randazzo, as well as Dr. Lipson and Dr. Nair.
With offices in Paramus, Union, Florham Park, Hazlet, and New York City, IGEA offers comprehensive, multi-disciplinary care to patients experiencing a wide variety of neurologic and musculoskeletal conditions and complaints.